All About…ATRIAL FIBRILLATION
AKA
AF as it’s colloquially known. AF+RVR is normally known as Fast AF.
Why?
Long-term AF: permanent changes in the structure of the atria caused by anything from valve issues, hypertension or ischaemia.
Temporary AF: alcohol, hormone imbalance, infection.
How?
Lots of electrical impulses, normally centrered around the pulmonary veins in the left atrium, fire at random causing the atria to fibrillate rather than fully contract.
There are three main types
1. Paroxysmal – the Come-and-Go version. Normally 24-48 hours, can be up to a week. Episodes happen infrequently and normally go without treatment.
2. Persistent – longer than a week. Normally needs treatment.
3. Permanent – no further treatments are attempted. You’re stuck with it.
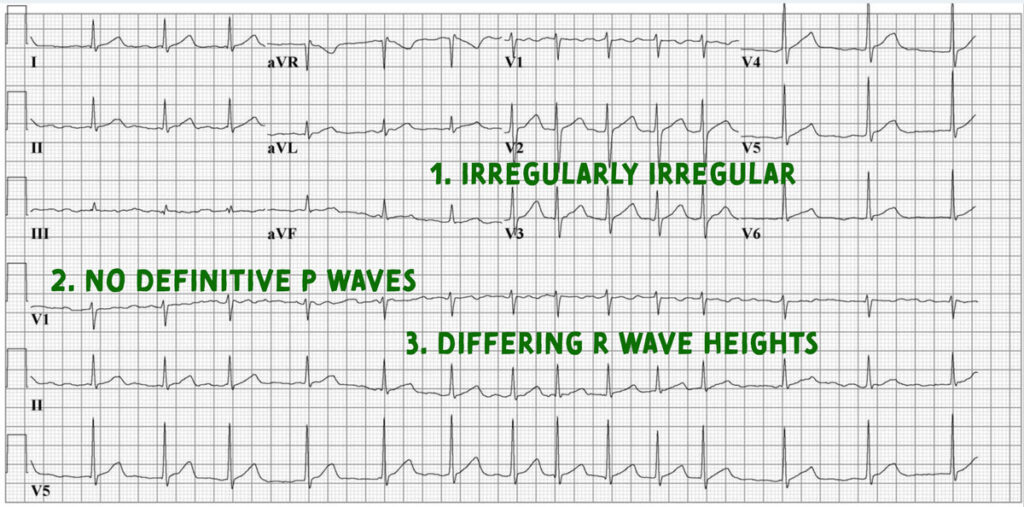
Lets look at the ECG….
The three distinctive features of AF on the ECG are:
What kind of patients?
Normally over 60 years of age, the older you are, the more likely it is you’ll have AF: you’re four times as likely to have AF in your 80’s than your 60’s.
So when do I need to be concerned?
Patients with AF are 5 times more likely to have a CVA so look out for any embolic phenomenon like CVA’s, DVT’s , PE’s.
When should I blue in AF?
The heart rate normally sits around 60-100bpm. Anything above 100bpm is called Atrial Fibrillation with Rapid Ventricular Response (AF+RVR) or more commonly Fast AF.
All about…FAST AF
Typically if the patient’s heart rate goes above 100, the ambulance service doesn’t know until it becomes quite rapid. Auntie Esther is not really going to note any large symptomatic changes if her heart rate goes from 90 to 110. However if her heart stays in Fast AF at a rate of 150-170 then she may feel unwell and dial 999. Therefore we tend to see faster versions of Fast AF on the frontline.
Auntie Esther will commonly feel palpitations (the fast irregular beat), lethargy / dizziness (reduced 02 in blood) and chest pain (from any ischaemia).
Atrial Kick is the amount of blood that the atria push through to the ventricles – about 20% with gravity and pressure doing the rest. Fast AF severely reduces Atrial Kick – but – as it was only 20% in the first instance the symptoms Auntie Esther experiences will be milder than a nasty heart block or say an MI that has taken out the SA node. Therefore Auntie Esther is more liley to experience the milder symptoms of say dizziness, light-headedness than a full-on T-LOC. If Atrial Kick was responsible for say pushing 80% of blood through to the ventricles, no doubt it would be classed in the same way as VF and we’d be shocking poor Auntie Esther who’d now be in cardiac arrest!
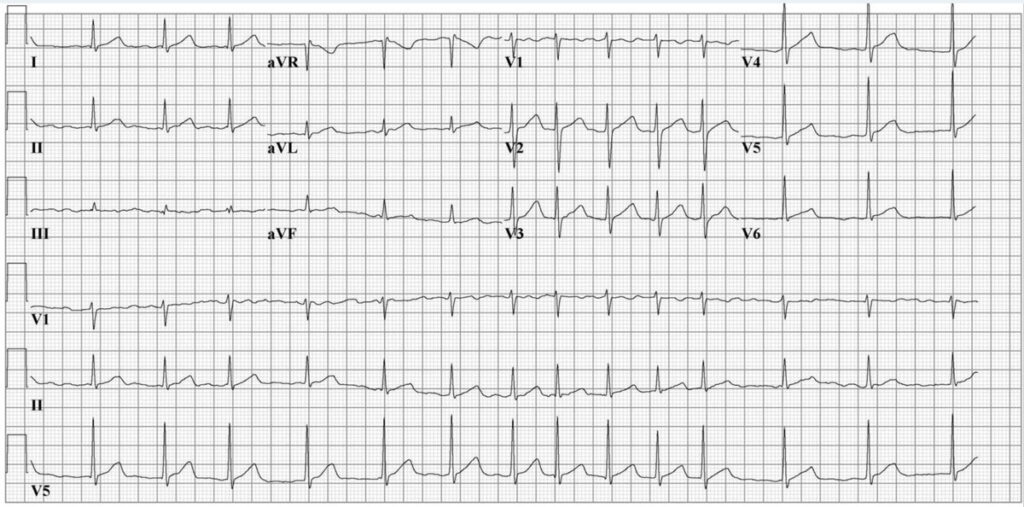
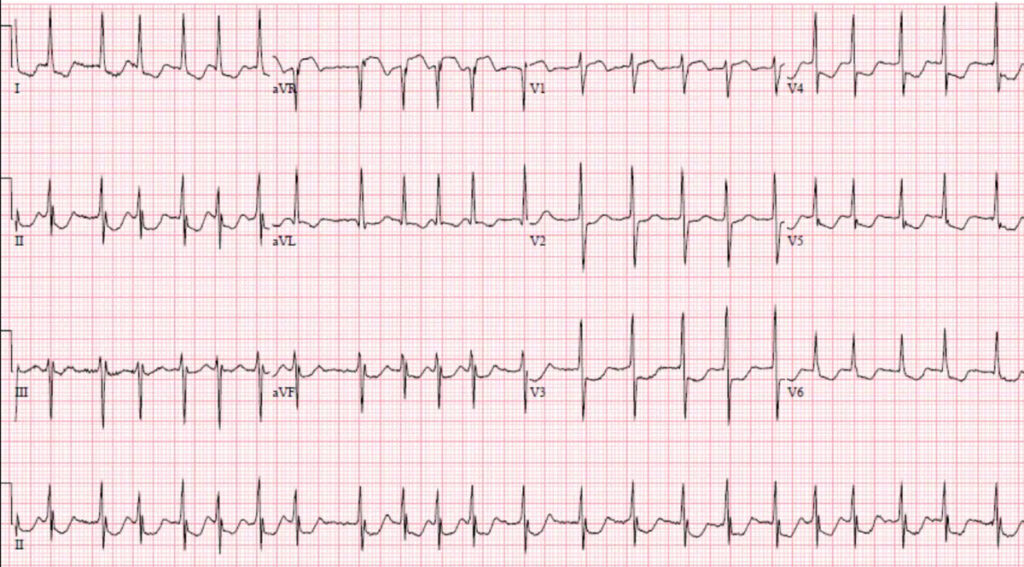
Here’s a Fast AF ECG:
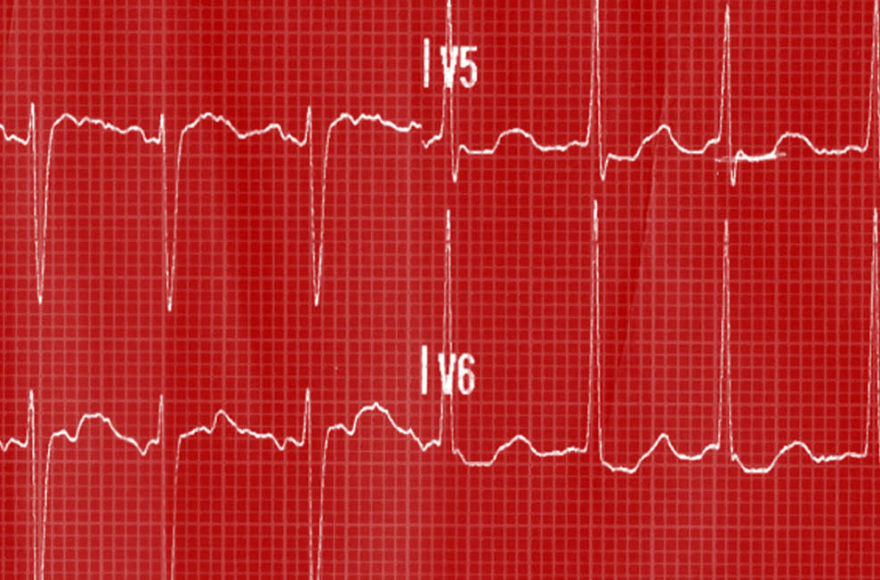
The reduced atrial kick plus the faster overall heart rate means the leisurely filling time the ventricles normally have is gone. Skipping a few chapters ahead, this means less 02 is getting to the heart muscle causing temporary demand ischaemia. You can see this below manifest on the ECG as depression:
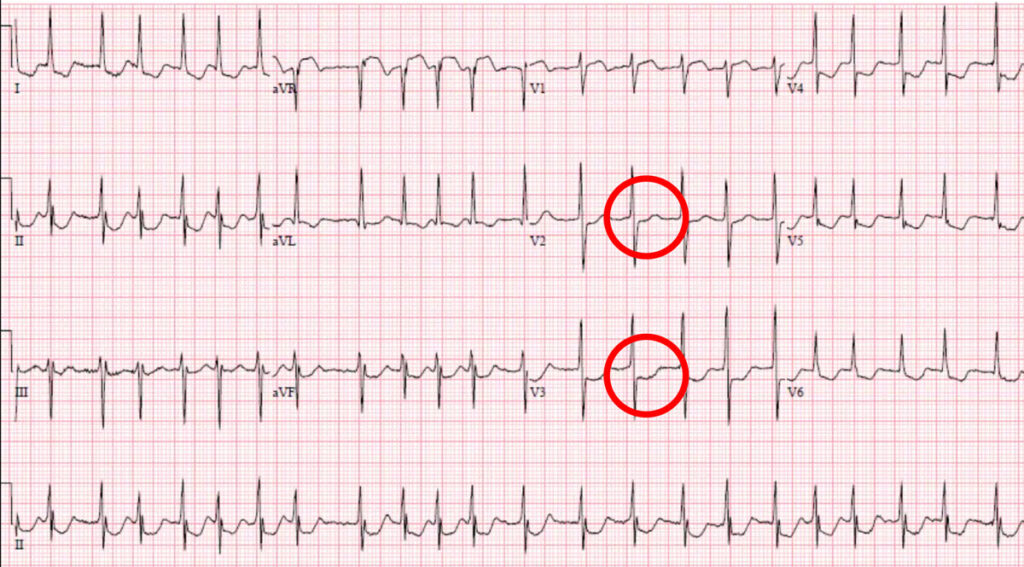
We would call this rate-related depression: as soon as the rate goes back to normal, the depression disappears. You don’t need to go to the cath lab or anthing in this situation – this is not acute coronary syndrome, this is temporary subendocardial ischaemia. Of course, caveat: be aware NSTEMI’s can present with AF so clinical judgement needs to be used!
So I blued my pateint in with Fast AF, now what?
Auntie Esther’s AF will probably be electically or chemically cardioverted – a crowd favourite in A&E is Metroprolol. Also if possible the underlying cause will be treated – giving ABX if the AF is induced by an infection for example.
References:
Wong, K., Ubogagu, E. and Francis, D. (2010) Cardiology to impress: The ultimate guide for students and junior doctors. London: Imperial College Press.