Bradycardia in an ESRF patient

A 43 yo male called as he felt a burning sensation in his chest, palpitations and his heart rate on his own sats probe showed 40bpm.
He confirmed a medical history of End-Stage Renal Failure (ESRF) and previous bradycardia. He had finished dialysis (x3 weekly) approx 4 hours previously. He also consumed a large pizza one hour prior.
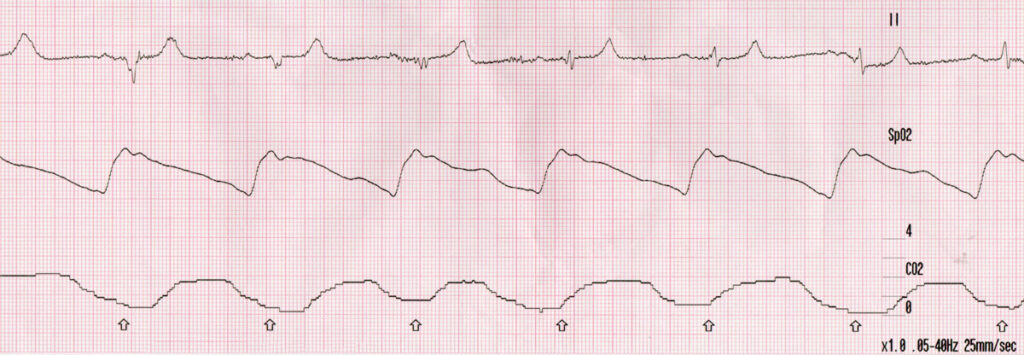
The patient was haemodynamically stable (BP 135/77) well perfused and not clammy, sweaty or pale. On arrival the ECG confirmed bradycardia:
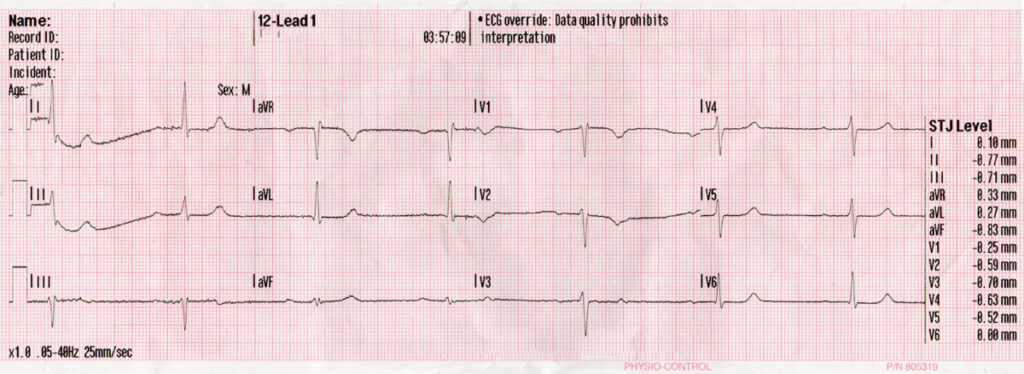
The rate was a consistent 40 with a prolonged PR and QT, flattened or non-existent p-waves and some PAC’s with compensatory pauses.
As seen above I didn’t think they weren’t PACs as I did not think there was any p wave hidden in the preceeding t-wave, there was an evident compensatory pause and the morphology was similar. I didn’t consider heart blocks as the pause wasn’t long enough to envelop a complete complex either.
So with these findings I assumed post-dialysis electrolyte imbalance, probably hyperkalaemia from a large postdialysis K+ bounce back. The patient mentioned the dialysis nurse had made a change from his regular treatment, but it was unknown what was changed.
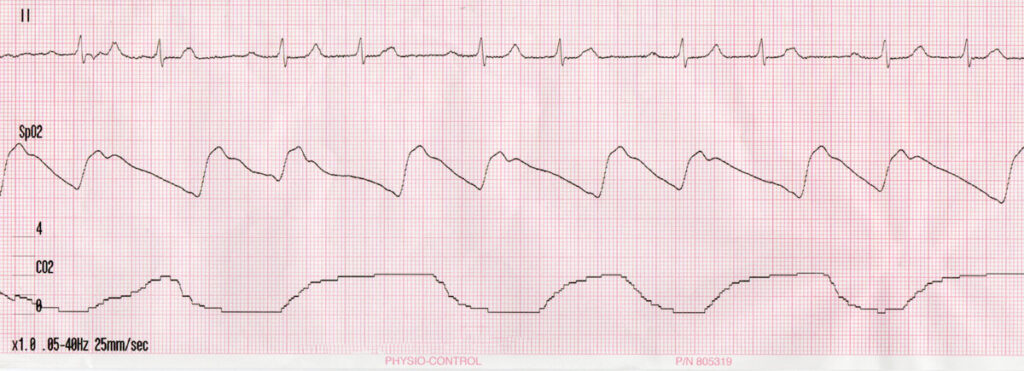
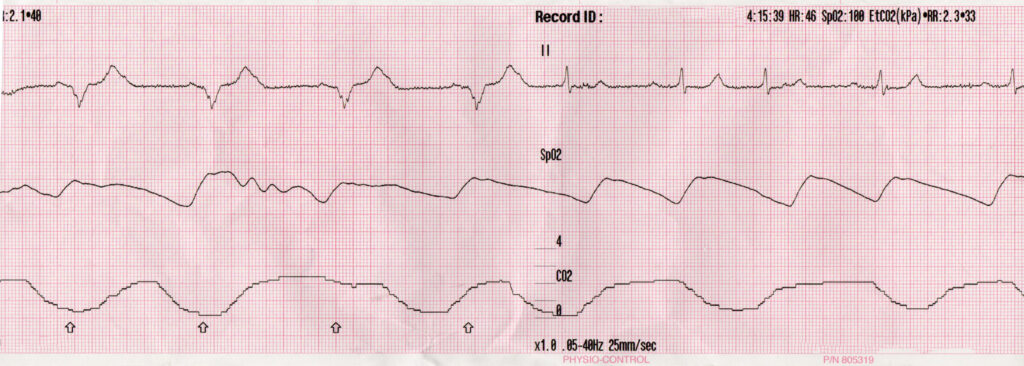
En route the patient’s rhythm suddenly changed as his heart rate went to 38bpm:
Initially on the monitor I thought this was sine wave pattern, however the patient remained unchanged, sat upright on the bed, talking. I noticed the pacing arrows. The patient then confirmed he had a pacemaker fitted as a result of a previous bradycardic episode, which he said, kicks in when his heart rate drops below 30 (I was thinking he was mistaken and it was 40). The rhythm then spontaneously reverted again after a few minutes and the pacemaker did not fire again.
The patient remained in stable condition en route and until handover.